NEW DRUG TO TREAT CORONAVIRUS
There Is A Drug Already Used In Japan Which May Treat COVID-19, Says New Study
A group of scientists in Germany have identified a drug called camostat mesylate, that they believe may work to combat COVID-19, the disease caused by the SARS-CoV-2 coronavirus.
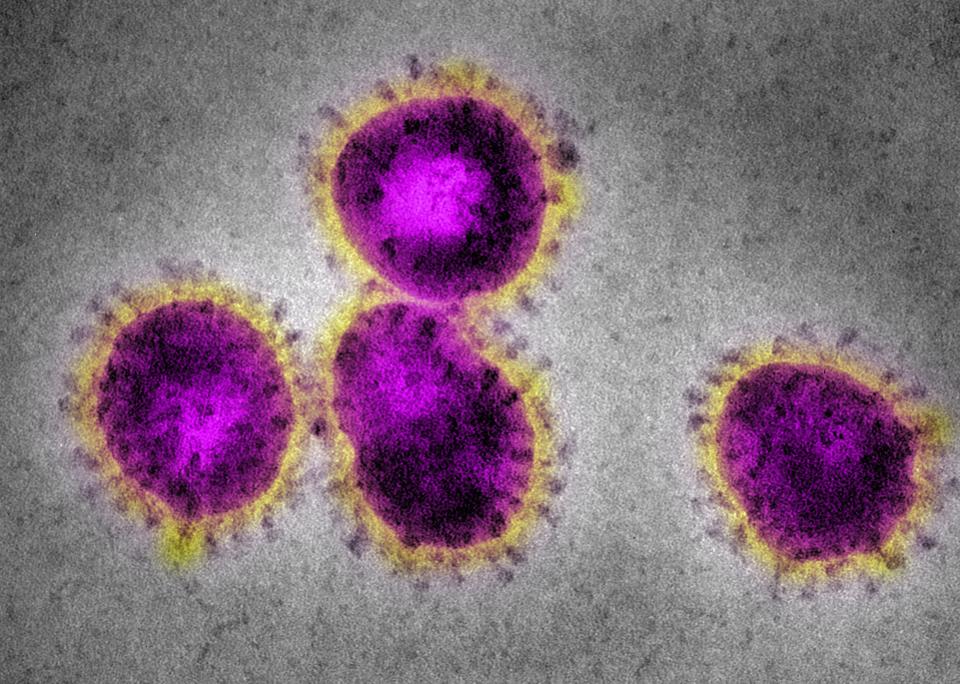
The new study published last week in Cell, shows that SARS-CoV-2 binds to human cells in a similar way to the original SARS coronavirus (SARS-CoV) that caused a worldwide outbreak in 2003, with this binding depending on viral proteins called ‘spike’ proteins.
“Spike is so named because that’s what it looks like: a spike on the surface of the virus particle,” said Angela L. Rasmussen, PhD, a virologist in the faculty of the Center for Infection and Immunity at the Columbia Mailman School of Public Health. “In order for a virus to infect a cell, it has to attach itself to a protein on the surface of that cell which we call the receptor. For SARS-CoV-2, this is a protein called ACE2. Spike binds ACE2 and allows SARS-CoV-2 to enter and infect cells,” she added.
As well as this initial process, the spike protein has to be primed by an enzyme called a protease in order for the virus to complete entry into the cell. The study showed that similar to SARS-CoV, SARS-CoV-2 uses a protease called TMPRSS2 to complete this process.
The scientists then looked at whether there were any compounds available that could stop the entry of coronavirus into the cell by stopping the TMPRSS2 protease from working. From previous work on SARS-CoV, they found one potential candidate called camostat mesylate and showed that the drug stopped SARS-CoV-2 from infecting lung cells in a dish.
“We found that SARS-CoV-2, like SARS-CoV, uses the host proteins ACE2 and TMPRSS2 to enter cells. Both viruses should therefore infect similar cells in patients and may cause disease via similar mechanisms,” said Markus Hoffmann, PhD, researcher in the Infection Biology Unit of the German Primate Center, Leibniz Institute for Primate Research, Göttingen, Germany and first author of the paper.
Developing new drugs for infectious diseases or even diseases such as cancer or neurological conditions can take years, even decades. But camostat mesylate has already been tested in people, albeit not for the treatment of COVID-19.
“We knew from our previous work that camostat mesylate was active against other coronaviruses, including SARS-CoV. Therefore, we tested whether it is also active against SARS-CoV-2,” said Stefan Pöhlmann, PhD, Professor in the same institute in Göttingen. “Our study shows that camostat mesylate blocks infection of cells with SARS-CoV-2-like particles and with authentic, patient-derived SARS-CoV-2. Moreover, camostat mesylate inhibited infection of important target cells – human lung epithelial cells,” he added.
The compound is approved in Japan for the treatment of a number of non-infectious conditions in people, such as chronic pancreatitis and postoperative reflux esophagitis and has also had some tests in mice infected with SARS-CoV. However, it has never been tested in humans with COVID-19.
“It does require trials in humans to determine if it’s effective, and I suspect it would also require pre-clinical animal work with SARS-CoV-2 specifically before human trials could start. If it has been shown to be safe for clinical use in other countries, it may be fast-tracked for FDA approval or the FDA may authorize emergency off-label use,” said Rasmussen, indicating that the FDA will have to examine safety data and pre-clinical data before determining which, if any course of action to take with investigating the drug further.
One concern is that TMPRSS2 might not be the only protease that controls spike priming and hence blocking it may be ineffective in people as other proteases may act as backups, still allowing the virus entry into cells. There are also questions to be asked about how the drug would actually alter the ability of the virus to cause disease in people.
“Pathogenesis can’t be studied in cultured cells, so these questions will need to be addressed using animal models and human clinical samples,” said Rasmussen.
Given the similarities between SARS-CoV and the current virus SARS-CoV-2, the researchers also looked at whether people who recovered from SARS had any immunity to the new virus strain. They took serum containing antibodies taken from 3 recovering SARS-CoV patients back around the time of the original outbreak in 2003 and showed that this blocked entry of SARS-CoV-2 into cells. The serum was taken from patients b
“Antibodies from patients who had recovered from SARS blocked the SARS-CoV-2 from infecting cells in culture. This suggests that antibodies against SARS might be useful as a treatment for SARS-CoV-2,” said Rasmussen.
SARS in 2003 was a smaller outbreak compared to the current situation with only 8,098 cases formally recorded and over 7,000 people surviving. It is not known how many of these people are still alive today, but it is possible that they will have some immunity to COVID-19. On a wider scale, studying these people may provide incredibly useful clues about successfully treating COVID-19. So, what are the next steps for the researchers?
“We are currently analyzing whether camostat mesylate-related inhibitors show improved antiviral activity. So far we have not been contacted by others regarding off-label use of camostat mesylate. However, we are contacting physicians to discuss this option,” said Pöhlmann.
There are currently no FDA-approved treatments for COVID-19, but last week, the National Institutes of Health announced that the antiviral drug remdesivir had begun testing in a human clinical trial in the U.S. Remdesivir, marketed by Gilead Sciences has previously shown promise in preventing MERS coronavirus disease in tests on monkeys and is already being used in human trials in Wuhan. The first patient in the U.S. is an American who was evacuated from the Diamond Princess cruise ship, which became a floating incubator for the virus, resulting in over 700 infections and six deaths reported so far.